Low back pain is probably the most frequent reason to visit doctors around world. In India patient loves taking pain killer without knowing the reasons for such pain. Many patient’s keeps on taking medicine for ages with little knowledge of harm it is doing to them. Chronic low back pain is neither a simple disease nor has simple solution. We would advise to take expert opinion on diagnosis & then start treatment as a small muscular sprain may be just a symptom of underlying serious disease.
Pain may arise from damage or irritation to structures of the lower back including the vertebrae (bony spine), facet joints, discs between the vertebrae, vertebral ligaments, muscles of the lower back, spinal cord and peripheral nerves. Thus it is of immense importance to understand & find the reason for such pain, which may be as small as muscular sprain or big as disc or nerve problem.

We have broadly divided treatment options into conservative management, image guided interventions, minimally invasive spine procedures & surgery depending upon specific diagnosis .
1.Conservative treatment: Consists of medication & exercises after confirming the problem to be myofascial.
2.Interventions: Image guided interventions are disease specific & done to reach to source of pain under live x-ray or ultrasound
3.Minimally invasive spine treatment: Instead of open spine surgery modern technique and equipments used to address the problem without destruction or destabilizing spine.
4.Open spine surgery: Surgical advise is only given when other modality fails or there are severe complications characterized by bladder and/or bowel incontinence, lower extremity weakness, spasticity, and/or loss of sensation.
Conservative management :
• Medications – NSAIDs (Ibuprofen like drugs), Acetaminophen (Tylenol), muscle relaxants, and membrane stabilizing medications are often effective in treating low back pain.
• Cryotherapy – A probe is placed through a needle near affected painful nerves. Electrical stimulation is done to verify position and freezing cycles are initiated over the painful nerves.
• Transcutaneous Electrical Nerve Stimulation (TENS) – is a technique that relieves pain by applying mild electric current to the skin at the site of the pain. The electric impulses interfere with normal pain sensations and alter perceptions that were previously painful.
• Biofeedback – is a treatment that teaches a patient to become aware of processes that are normally thought to be involuntary inside of the body (such as blood pressure, temperature and heart rate control). This method enables you to gain some conscious control of these processes, which can influence and improve your level of pain. A better awareness of ones body teaches one to effectively relax and this can help to relieve pain.
• Physical therapy – In order to decrease or prevent functional limitations, physical therapy and occupational therapy are recommended as well as medical treatments.
Interventions:
• Epidural intervention – Epidurals are frequently used for pain syndromes due to common conditions such as degenerative disc disease. The method involves injecting a anti inflammatory medicine into the epidural space of the spine, where the irritated nerve roots are located. The medicine then spreads to other levels and portions of the spine, reducing inflammation and irritation.

• Medial Branch Blocks/Denervation – Medial Branch Blocks (MBBs) are a minimally invasive non-surgical treatment that are used for arthritis-related neck and back pain. The injections work by reducing the inflammation and irritation in the facet joints of the spine that is causing your pain.
• Lysis of Adhesions – Also known as the “Racz Procedure,” this procedure has proven effective in removing excessive scar tissue in the epidural space when conservative treatment for lower back pain has failed. A study performed in 2005 said, “a spinal adhesiolysis with targeted delivery of local anesthetic and medicine is an effective treatment in a significant number of patients with chronic low back and lower extremity pain without major adverse effects.”
• Infusions Techniques – The procedure involves inserting a small catheter through a needle into the epidural space or directly next to affected nerves. Local anesthetic and other medicines are often given through the catheter for extended time periods. When the nerves are blocked continuously with an infusion, pain relief can be dramatic and long lasting.
• Peripheral Nerve Blocks and Ablation – Nerves away from the spinal cord are called peripheral nerves. These nerves can often be sources of pain and can be blocked with local anesthetic. When pain relief is obtained, ablation or destruction can be initiated.
• Trigger Point Injections – can be an effective treatment for muscle spasms. The procedure involves injecting a local anesthetic and anti-inflammatory medication into a “Trigger Point.”
Minimally invasive spine treatment
• Endoscopic discectomy – is a minimally invasive spine procedure, which allows us to treat any problematic disc more safely with great success rate than open spine surgery. Endoscopic discectomy has proved of value not only for discectomy but also for many other back problems. With this minimally invasive technique all kinds of back & neck pain can be addressed in a very tissue-preserving way.
• Endoscopic Foraminotomy – is a minimally invasive spine procedure used to relieve pressure to spinal nerve roots, caused by compression from bone spurs, disc herniations, scar tissue, or excessive ligaments.
• Endoscopic facet rhizotomy – an advanced minimally invasive spine procedure alleviating pain coming from facet joint syndrome or spine arthritis.
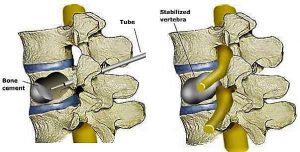
• Kyphoplasty and Vertebroplasty – are both minimally invasive procedures that can treat osteoporotic fractures. The method is to stabilize crushed vertebrae by injecting an acrylic cement into the vertebra. Vertebroplasty is effective in relieving pain, most likely because of the added support and stability it provides the spine.
• Spinal Cord Stimulation (SCS) – an implanted electrical device that decreases the perception of pain by confusing the spinal cord and brain pain processing centers. Initially, a trial is done to see if this device will help you long-term. In the initial trial, your pain physician places a small electrical lead in the epidural space through a needle. Painful signals are replaced by tingling electrical signals. If you have success in your trial, you may decide to have a permanent SCS device implanted.

• Peripheral Nerve Stimulation – this method involves tiny electrodes being placed close to the affected nerves. The electrodes release a small electrical current that inhibits pain transmission and causes pain relief.
• Intrathecal Pump Implants – Implanted pain pumps are also available which can be extremely helpful providing long-term pain control. The effectiveness of intrathecal therapy in patients suffering from nociceptive pain showed a pain reduction in 66.7% of patients experiencing pain due to cancer (Becker 2000).
• Nucleoplasty – Percutaneous Disc Nucleoplasty therapy is designed to reduce the tissue volume of the spinal disc by evaporating part of the liquid core, this lowers the pressure on the walls of the spinal disc, which in turn reduces the painful protrusion of the disc. The pain related to bulging spinal disc walls will subside after the procedure.
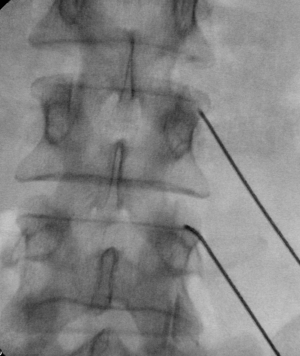
• Percutaneous Spine fixation with or without vertebral graft
There are many different minimally invasive spine procedures for back pain. The goal of nearly all procedure is to remove pressure from the nerves of the spine, stop excessive motion between two or more vertebrae or restores the function of spine. The type of Procedure that is best depends on that patient’s conditions and symptoms which requires comprehensive examination & unerstanding of disease.
Open Spine Surgery
Long-term, surgical fusion or discectomy may not provide relief. In addition, surgical options for LBP were found to be associated with a significant risk of complications, including bleeding, nerve damage, epidural scarring, and prolonged recovery times. The evidence at the present time does not support routine surgical fusion or surgery for the treatment of chronic lower back pain alone.There have been great strides in back pain treatments and interventional pain medicine. Early intervention can make a big difference.
Scientific publications:
o Early intervention for the management of acute low back pain: a single-blind randomized controlled trial of biopsychosocial education, manual therapy, and exercise. PMID: 15507794. Spine. 2004 Nov 1;29(21):2350-6.
o Surgical management of neck and low back pain. PMID: 17445741 Neurol Clin. 2007 May;25(2):507-22. Clinical Trials: 2007;10;425-440.
o Evaluation of Lumbar Facet Joint Nerve Blocks in the Management of Chronic Low Back Pain: Preliminary Report of a Randomized, Double-Blind Controlled Trial: Clinical Trial NCT00355914 Laxmaiah Manchikanti, MD, Kavita N. Manchikanti, BA, Rajeev Manchukonda, BDS, Kimberly A. Cash, RT, Kim S. Damron, RN, Vidyasagar Pampati, MSc, and Carla D. McManus, RN, BSN
o Surgical versus non-surgical treatment of chronic low back pain: a meta-analysis of randomised trials. PMID: 17119962 Int Orthop. 2006 Nov 21
o Physiotherapist-Directed Exercise, Advice, or Both for Subacute Low Back Pain: A Randomized Trial Liset H.M. Pengel, Kathryn M. Refshauge, Christopher G. Maher, Michael K. Nicholas, Robert D. Herbert, and Peter McNair Abstract for study: http://www.annals.org/cgi/content/abstract/146/11/787
o “Meta-Analysis: Acupuncture for Low Back Pain.” 19 April 2005 issue of Annals of Internal Medicine (volume 142, pages 651-663). E. Manheimer, A. White, B. Berman, K. Forys, and E. Ernst Summary of study: http://www.annals.org/cgi/content/summary/142/8/651
o A randomized, controlled trial of spinal endoscopic adhesiolysis in chronic refractory low back and lower extremity pain [ISRCTN 16558617] Laxmaiah Manchikanti1 BMC Anesthesiology 2005, 5:10 doi:10.1186/1471-2253-5-10
o Effect of periarticular and intraarticular lidocaine injections for sacroiliac joint pain: prospective comparative study. Murakami E, Tanaka Y, Aizawa T, Ishizuka M, Kokubun S. J Orthop Sci. 2007 May;12(3):274-80. Epub 2007 May 31 PMID: 17530380





